What to do if you’re depressed?
What is major depressive disorder (MDD)?
How to stop being depressed?
Depression can take many forms, however there are several consistent symptoms.
Mental health professionals use these symptoms and signs of depression, listed below, to determine whether someone is suffering from a depressed mood and/or major depressive disorder (MDD).
Some people who are depressed experience profound anhedonia—a loss of pleasure in everyday activities.
Americans’ Google searches for anhedonia have been growing over the past 18 years.
Others experiencing depression may not be fully aware of what’s going on and may attribute our experiences to a “low mood” or “feeling down.”
Whether we’re facing new challenges at work, tackling issues with family or conquering financial difficulties—feeling down, experiencing a low mood, or feeling anxious can be a normal human response to the wide array of stressors we all experience.
Feeling down can be a response to particular stressors and grief, however—in these cases—temporary low mood generally does not mean we are depressed.
But, what about if feeling down begins to take over and become something we are experiencing every day?
Or if anhedonia kicks in with full force, rendering us unable to enjoy our lives as we did before?
Does it mean we’re depressed? And, what exactly is depression, anyway?
Read on to find out the official signs and symptoms of depression, as well as the treatment, and how to get help if you think you might be depressed.

First, what’s depression? Is it the same as major depressive disorder (MDD)?
We may often characterize depression as a state of being in low spirits.
However, according to the American Psychological Association (APA) Diagnostic and Statistical Manual, fifth edition (DSM-5)—the handbook that provides guidelines for clinicians who diagnose psychiatric illnesses—a depression diagnosis requires five or more symptoms.
And one of the symptoms must be either depressed mood or anhedonia.
The official diagnosis of depression in the DSM-5 is called major depressive disorder (MDD).
Symptoms of depression and major depressive disorder (MDD)
While a low mood is associated with depression—that symptom alone isn’t enough to mean you could be diagnosed with major depressive disorder (MDD).
According to the DSM-5, to be diagnosed with depression or MDD, 5 or more of the following symptoms must be present during the same 2‐week period:
Depressed mood most of the day, nearly every day as indicated by either subjective report or observation made by others (for example, feeling sad, empty, hopeless)
Diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (also known as anhedonia) as indicated by either subjective account or observation
Significant weight loss (when not dieting on purpose) or weight gain (for example, a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day
Insomnia (having trouble sleeping) or hypersomnia (sleeping a lot more than usual) nearly every day. If you're wondering if you're depressed or just extra-tired, here are some ways to find out.
Psychomotor agitation or slowness nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down)
Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day
Diminished ability to think or concentrate, or indecisiveness, nearly every day
Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide
Depression can manifest in a number of ways, says physician Dr. Michael McGrath, M.D., assistant clinical professor at the University of Hawaii John A. Burns School of Medicine, who specializes in psychiatry, neurology, and addiction.
According to Dr. McGrath, symptoms of depression can include:
Mood changes, such as sadness or irritability
Changes in appetite
Drug or alcohol use
Feeling tired more than usual or having no energy
Having no motivation or enjoyment in normal activities (anhedonia)
Feeling hopeless
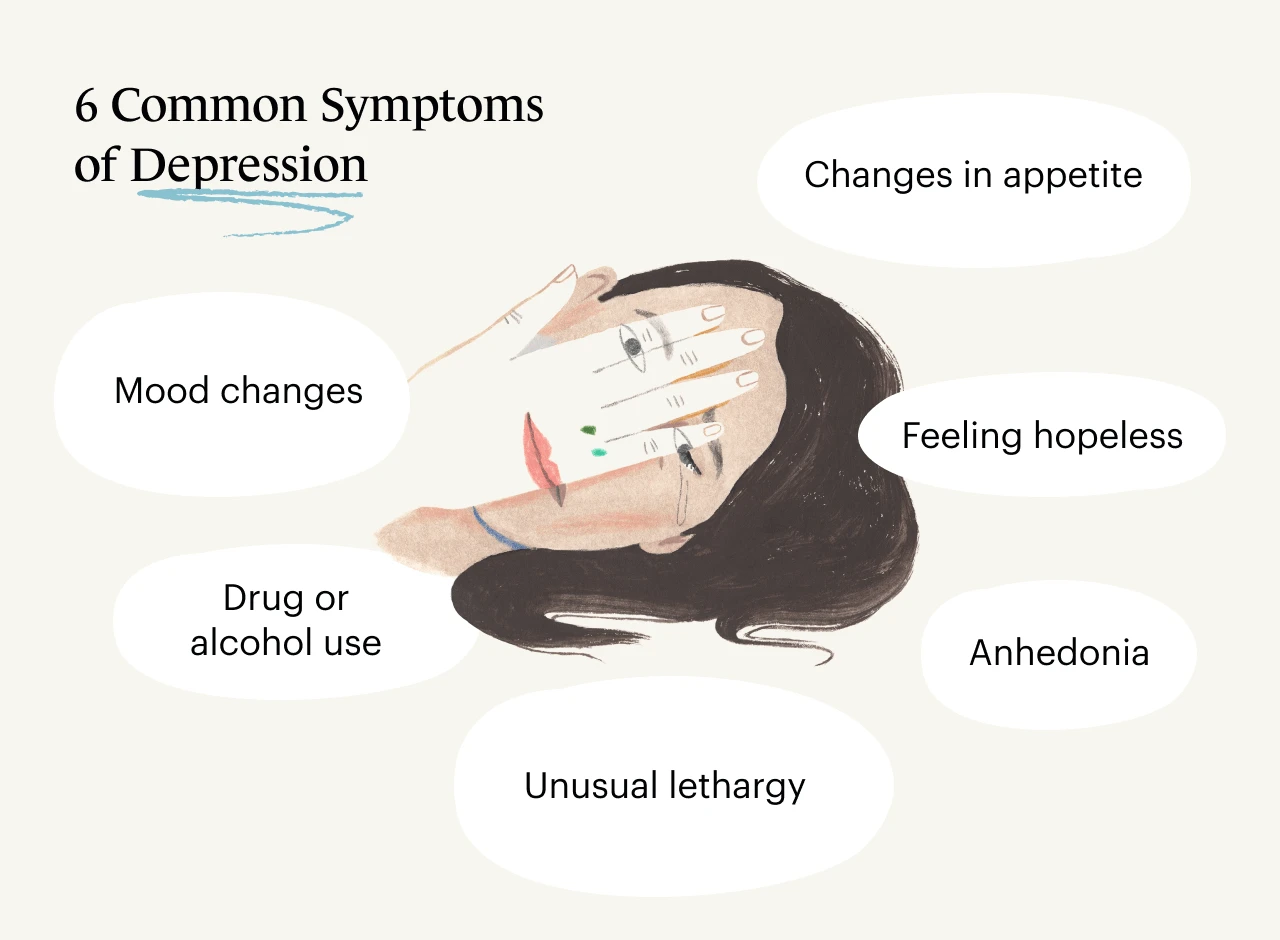
Dr. McGrath notes symptoms must present nearly every day and be present for at least a two-week period.
“Feeling sad one or two days out of a three-week period would not necessarily be a symptom of depression,” says Dr. McGrath. “But if it occurs every day during those three weeks, it could be.”
Licensed clinical psychologist Dr. Anton Shcherbakov, Psy.D, BCBA, a nationally recognized expert on mental health issues, adds that individuals who are depressed may also experience feelings of worthless/hopelessness, suicidal ideation, and difficulty with focus and concentration.
Depression can be even trickier to identify as symptoms can be so different from person to person.
Monarch therapist Saba Harouni Lurie, LMFT, owner of Take Root Therapy in Los Angeles, explains that while symptoms of depression can include hallmark traits like changes in eating or sleep, these can occur in varying degrees for different people.
“Some people who experience depression may sleep more than they usually would, while others may have a difficult time falling and/or staying asleep," says Lurie.
"Similarly, some who experience depression may eat beyond feeling satiated, while others may lose their appetite completely,” she explains.
How many Americans have depression?
According to the National Institute of Mental Health (NIMH) 2020 National Survey on Drug Use and Health, 21 million adults had at least one major depressive episode in 2020.
That’s 8% of all American adults.
The percentage was higher among women—with 10% of females experiencing depressive episodes, compared to 6% in males.
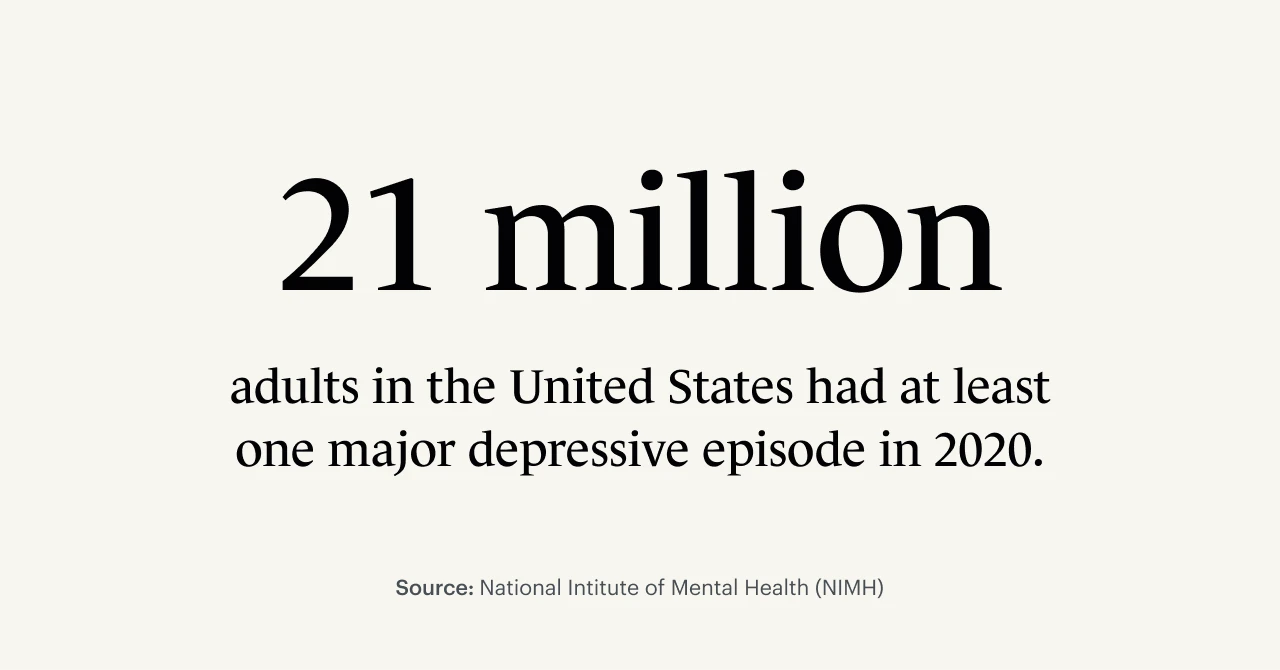
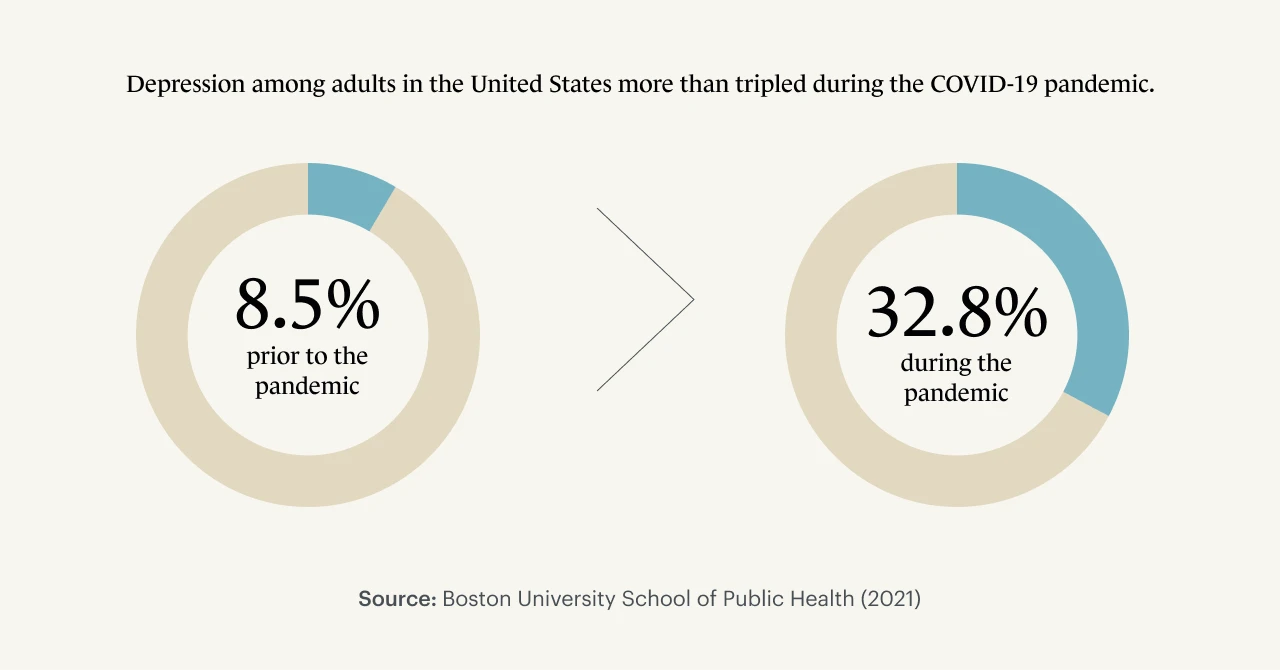
It’s also worth noting these numbers have significantly risen in the last year due to the COVID-19 pandemic trauma, with depression rates tripling at the pandemic's onset.
New research from Boston University School of Public Health reveals that the elevated rate of depression has climbed to 33%, affecting one in every three American adults.
The study also explained that the most significant predictors for adults experiencing depressive symptoms included low income, not being married and facing other pandemic-related stressors.
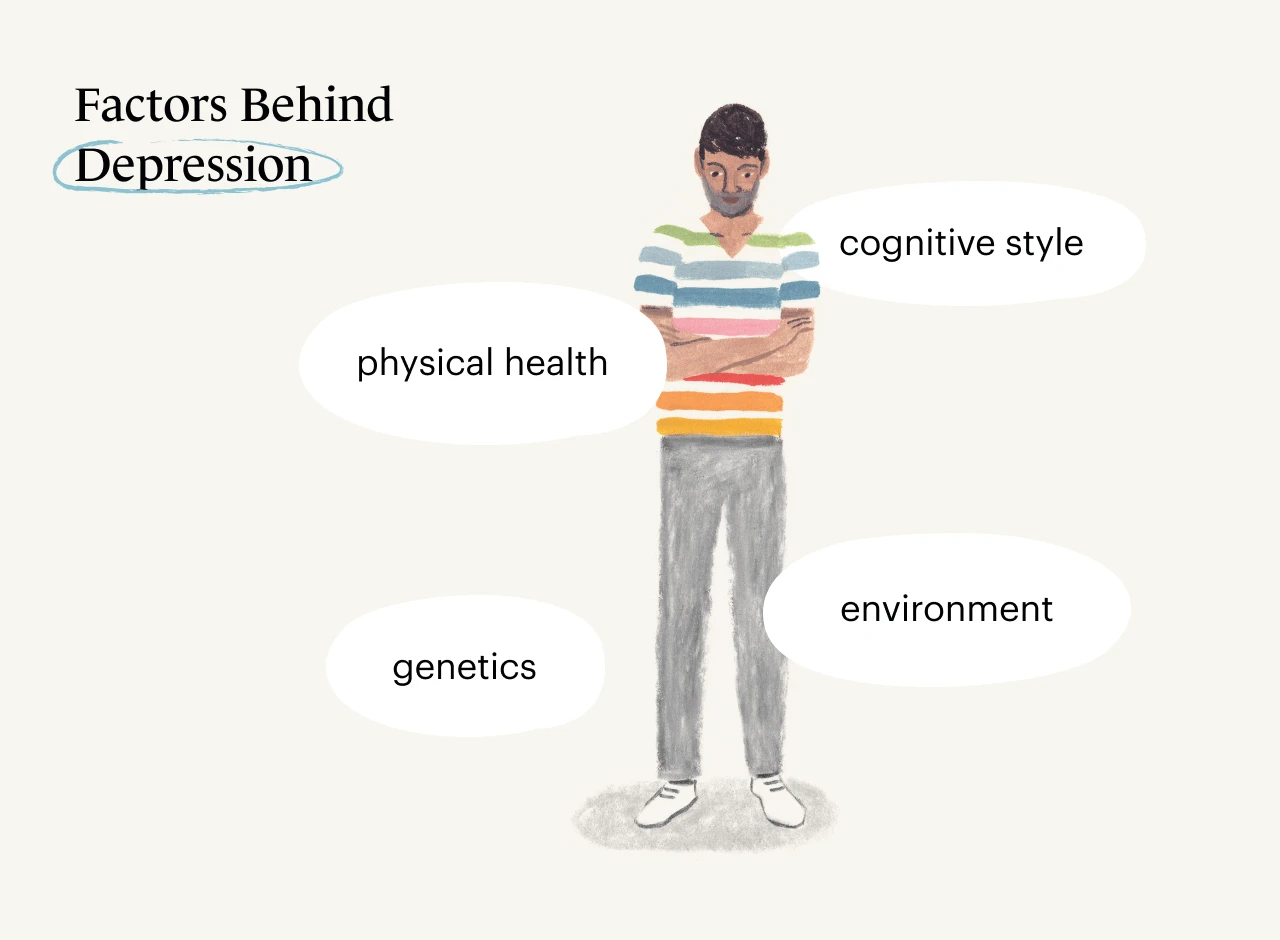
Where does depression come from?
We know that four key players–serotonin, dopamine, norepinephrine and glutamate–are neurotransmitters in our brains implicated in depression and mood disorders.
But simply blaming these four neurotransmitters is not enough to give us a the entire story on the causes of depression.
According to Dr. Shcherbakov, “Genetics, physical health, cognitive style, and environment all contribute to depression.”
He points out that certain individuals may be more susceptible to depressive episodes because of their genetic family history, for instance.
“Others with poor physical health–such as those with cardiovascular diseases–are also significantly more susceptible to experiencing a depressive episode,” says Dr. Shcherbakov.
Some of the root causes of depression are also attributed to maladaptive cognitive styles: individuals who are more pessimistic or ruminate excessively are more likely to experience a depressive disorder in their lives.
“Although it seems that our emotions and motivations result directly from the events and circumstances we encounter, they are instead reactions to our self-talk," says retired clinical psychologist Dr. John F. Tholen, Ph.D., author of Focused Positivity: The Path to Success and Peace of Mind, "the internal monologue that streams endlessly through our waking consciousness, interpreting whatever we experience.”
Poor social support systems, unhealthy environments and high levels of stress can also contribute in a significant way.
Trauma and grief are also implicated as potential root causes; adverse life experiences, including Adverse Childhood Experiences (ACES), are more prone to depressive symptoms, says Monarch therapist Alisa Kamis-Brinda, LCSW, LCADC, owner of Serenity Solutions, LLC.
What’s depression doing in our bodies and brains?
“Depression is a complex condition characterized by both cognitive and biochemical changes,” says Dr. Shcherbakov. “On a biochemical level, any number of neurotransmitters may be impacted, including serotonin, glutamate, norepinephrine, and dopamine.”
Serotonin is a neurotransmitter involved in regulating mood, cognition, reward, learning, memory.
Dopamine is another neurotransmitter that plays a huge role in how we feel pleasure.
Norepinephrine is a hormone and neurotransmitter crucial to maintaining our bodies’ responses to stressors, aka the fight-or-flight response.
Glutamate is an amino acid that functions as an excitatory neurotransmitter.
All four of these compounds play vital roles in how our bodies respond to stress.
According to Dr. Shcherbakov, a growing body of research shows that these changes in chemistry and cognition may lead to behavioral symptoms of depression that we can observe externally, such as deceased pleasure-seeking activity and withdrawal from support symptoms.
These new behavioral changes may then, consequently, maintain and exacerbate our feelings of depression.
Treatment for depression and mood disorders
“Because the causes of depression are complex, the treatments for depression are usually most effective when they are multi-modal,” explains Dr. Shcherbakov.
He recommends patients begin by addressing any physical health issues that may exacerbate their depressive episodes.
These can include poor sleep or a bad diet with a lack of nutrition.
Getting regular exercise, such as a daily walk, can also be helpful for those experiencing mild or moderate depressive symptoms.
The most successful evidence-based treatment for depression, however, is a psychological approach known as Cognitive-Behavioral Therapy (CBT).
Tholen points to a comprehensive review of 325 different research studies involving more than 9000 subjects that found CBT significantly improved depression in adults and adolescents.
“CBT relieves depression by challenging underlying dysfunctional thoughts—those that cause distress without inspiring constructive action,” says Tholen.
Other therapy styles that have been shown by research to be effective in helping with depression include Acceptance and Commitment Therapy (ACT) and Dialectical Behavior Therapy (DBT).
Medication is commonly thought of as a first line treatment for depression in the media–this is far from observed practice.
Dr. Shcherbakov points out that while medication such as SSRIs (selective serotonin reuptake inhibitors) and SNRIs (serotonin and norepinephrine reuptake inhibitors) may be a helpful adjunct treatment to depression, these medications should not be the sole means through which people seek to treat their depressive episodes.
“Relying solely on medication does not allow people to address the other systemic factors that often maintain depression (e.g., lack of social support, poor working conditions, cognitive pessimism),” Shcherbakov says.
“That said, if medication alone is the only option, it is better than no treatment at all,” he concludes.
Medications used to treat depression include SSRIs, such as Prozac and Paxil, and SNRIs, such as Lexapro, Cymbalta, and Celexa.
“For people who have treatment-resistant depression, where many medications have been tried but have not been successful, TMS (transcranial magnetic stimulation) and ECT (electroconvulsive therapy)are helpful options,” Kamis-Brinda adds.
Other treatments for depression include psychotherapy, also known as “talk therapy,” and specifically cognitive behavioral therapy (CBT) in which therapists aim to help a person identify and challenge dysfunctional thought patterns and automatic negative thoughts.

Still wondering if you're depressed? Take our online depression assessment
If you’re concerned you might be depressed, take our online depression assessment to receive immediate feedback about whether you may be experiencing a depressive disorder.
It's fast, free, confidential, and clinically validated.
How and when to find help
If you suspect you might be depressed, it’s important to reach out to a doctor or mental health professional, such as a therapist.
“Seek out help if your symptoms are interfering with daily functioning, your work, or your relationships in significant ways,” recommends Kamis-Brinda.
The Monarch Directory by SimplePractice can connect you with therapists who specialize in treating depression.
You can quickly and easily view their availability and book a therapy session. Many therapists on Monarch offer free 15-minute initial consultations and in-person or telehealth video therapy sessions. If you have health insurance coverage, you can also browse therapists who accept your insurance.
Remember, if you or a loved one is suffering from mental health issues, you are not alone.
Here are some additional resources that can help:
The National Suicide Prevention Hotline is toll-free, 24/7 support. The phone number is 1-800-273-8255.
The National Alliance on Mental Illness provides information and support for those who suffer from mental illness, and their families and caretakers.
The Suicide Awareness Voices of Education(SAVE) foundation provides resources for those who have survived a loss by suicide.
READ NEXT: What Are the Types of Depression and the Levels?
Need to find a therapist? The Monarch Directory by SimplePractice can help you find licensed therapists near you who specialize in treating depression.