On my drive toward Boston I listened to my favorite podcast, Terrible, Thanks for Asking, hosted by Nora McInerny.
During this particular segment, her guest mentioned a term I’d never heard before: Adverse Childhood Experiences (ACEs). He explained that ACEs are potentially traumatizing events that occur throughout childhood (defined as ages 0-17) and can be linked to any number of troubles later in life.
ACEs can contribute to everything from chronic health problems to mental illness and substance misuse in adulthood; they can even negatively impact one’s education and job opportunities.
What is trauma?
No one had a perfect childhood. That goes without saying. But what counts as trauma?
According to the American Psychological Association, "trauma is an emotional response to a terrible event, or series of events, such as childhood neglect, an accident, assault, rape, or natural disaster. Immediately after the event, shock and denial are typical, but longer-term reactions include unpredictable emotions, flashbacks, strained relationships, and even physical symptoms like headaches or nausea.”
While I couldn’t point to any one discrete incident as “the” trauma of my childhood, I had been and still am struggling with chronic pain for much of my adult life.
Could that be a sign of childhood trauma? How could I find out?
The ACE assessment
It turns out there’s a 10-question assessment to help identify the extent of ACE factors in your life. It's based on a large-scale research study conducted by the CDC and Kaiser Permanente that found a connection between ACEs and health and social problems.
The short assessment asks a variety of questions such as whether your parents got divorced, and if an adult was abusing alcohol or drugs while you were growing up.
At the end, it gives you a score between one and ten. As you might assume if you score one you have very few ACEs with long-term effects on your physical and mental health. The closer you are to ten, the higher your chances are of these issues showing up later in life.
A few days after hearing the term “ACE” for the first time, I took the test. I am a six. Seeing that number flash up on the screen, bold and blue, I was stunned.
“I’m a six,” I said to myself quietly. As I sat at my kitchen counter that lazy Saturday afternoon it was only then that I was finally able to admit the truth: I am a survivor of childhood trauma.
While I couldn’t point to any one discrete incident as “the” trauma of my childhood, I had been and still am struggling with chronic pain for much of my adult life.
It’s not that I had been totally oblivious to my childhood experiences up to this point. Quite the opposite. I have been in and out of therapy with and without my family since I was around nine or ten years old. I know the damage they caused. I know how I’ve struggled because of it: in my marriage, with friends, and in work situations. I just didn’t know what to do about it.
Curious about your own ACE score?
Take the Adverse Childhood Experiences (ACE) assessment today to get your ACE score. It's free and only takes 3 minutes to complete.
When to call for backup
By 2019, it had been 15 years since I’d started seeing my therapist. I really liked her, she seemed to really like me, and she knew the full cast of characters. After that amount of time, it’s hard to think about picking up and starting over, yet I began questioning why I wasn’t making more progress.
I don’t mean to insinuate that my therapist was supposed to “cure” me but after all that time I still didn’t feel like I had the tools I needed to handle the rough waters when certain situations arose.
After talking about it with a family friend, who is also a therapist, it became clear that I needed someone who could really focus on helping me explore the trauma I suffered as a child. I needed trauma-focused therapy.
What is trauma-focused therapy?
Even as a therapy veteran, I had no idea there was a difference between “regular” therapy and “trauma-focused” therapy. Northwestern University’s Center for Child Trauma Assessment, Services, and Interventions defines “therapy” as something that provides “a safe and confidential place for a person to talk to a professional about personal experiences, thoughts, feelings, or problems.”
I still didn’t feel like I had the tools I needed to handle the rough waters when certain situations arose.
“Trauma-focused” therapy, then, is a “specific approach to therapy that recognizes and emphasizes understanding how the traumatic experience impacts a child’s mental, behavioral, emotional, physical, and spiritual well-being,” and ultimately affects their lives as adults.
This type of therapy is rooted in understanding the connection between the trauma experience and the person’s emotional and behavioral responses.
Like all therapy, there is no right or wrong type of trauma-focused therapy. The approach, also called an “intervention,” depends on what happened, the person’s age, and a whole variety of other extenuating factors.
These individually designed treatments can include everything from cognitive-behavioral therapy to Trauma Assessment Pathway to Attachment, Self-Regulation, and Competence. There are even interventions focused on mindfulness as a tool for helping patients manage their anxiety, among many more.
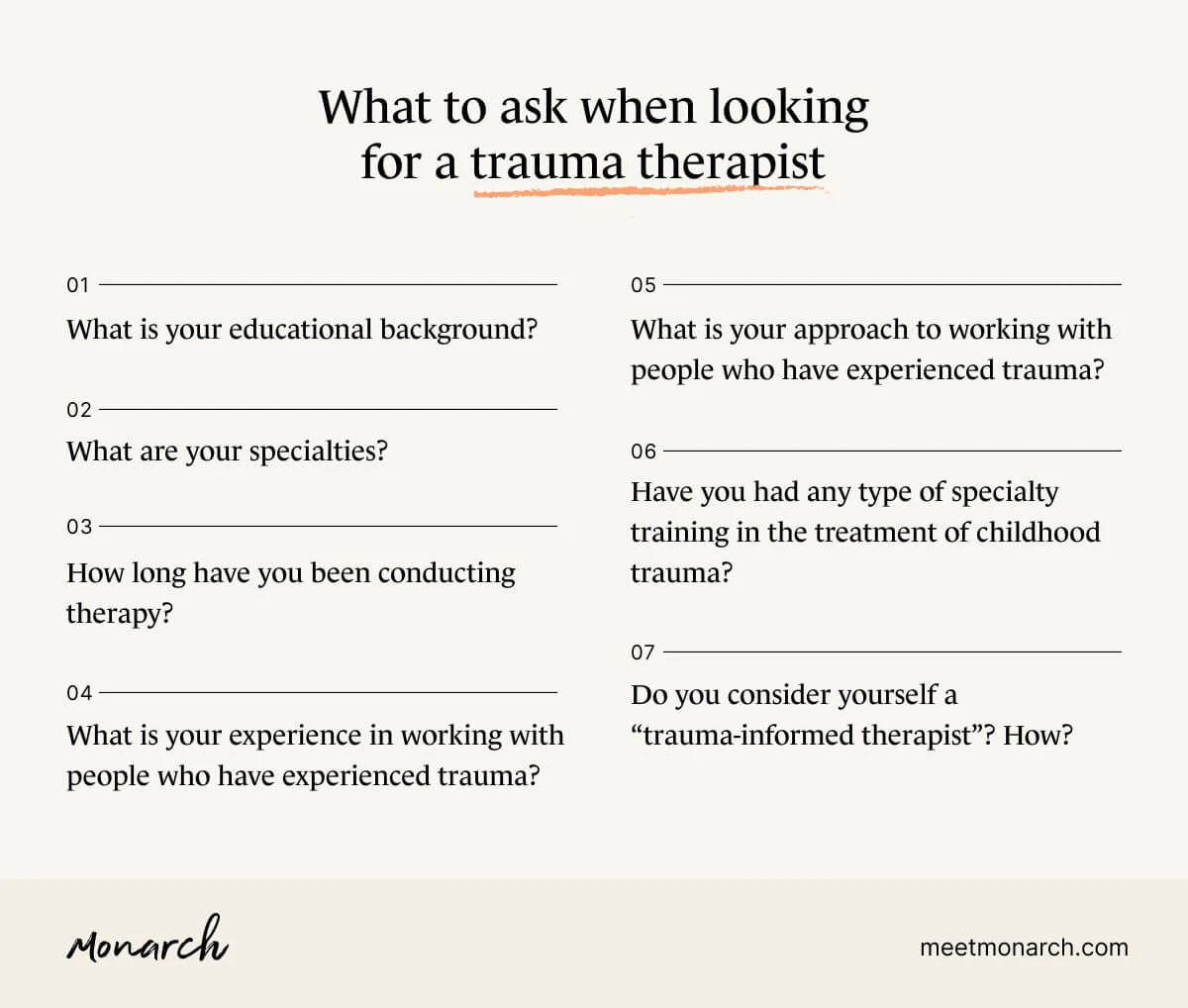
What to ask when looking for a trauma therapist
With no state or national regulations defining “trauma-informed provider” or “trauma-informed therapist” currently, here are some helpful things to ask when looking for a trauma therapist, according to Northwestern:
What is your educational background (degree, professional title)?
What are your specialties?
How long have you been conducting therapy?
What is your experience in working with people who have experienced trauma?
What is your approach to working with people who have experienced trauma?
Have you had any type of specialty training in the treatment of childhood trauma?
Do you consider yourself a “trauma-informed therapist”? How?
In order for you and your therapist to be as effective as possible in achieving your mental health goals, it’s incredibly important to be brutally honest about what happened, when it happened, and how it made—and makes—you feel.
Without that transparency, it’s impossible for your therapist to do a complete assessment and determine which style of trauma-focused therapy is best for you and your recovery.
Be gentle with yourself as you move through the process of finding the best fit for you.
No matter how hard you search and how much research you do, keep in mind that finding a therapist who you are comfortable with is essential. You’ve done the hardest part by identifying you have trauma that needs to be addressed. Be gentle with yourself as you move through the process of finding the best fit for you.

I found my trauma therapist based on a recommendation from a friend, which isn’t always the best way to find a therapist. But she was the perfect therapist for me. She and I are both trained in reiki (an energy-based healing technique) so right away we had a shorthand as we discussed my issues.
She was tough, she was blunt, but she was also the best person to help me move past the challenges I faced. I’m a person who believes people come into your life exactly when you need them—even if you don’t think you’re ready. We came to each other so serendipitously that I knew it was time to take the leap, and I’m so glad I did. Finding a therapist who specializes in trauma-informed therapy to talk with may help.
Need to find a therapist near you? Check out the SimplePractice Monarch Directory to find licensed mental health therapists with availability and online booking.
Adverse childhood experiences (ACEs). (2020). Retrieved from https://www.cdc.gov/violenceprevention/aces/index.html
APA. (2020). Trauma and shock. (2020). Retrieved from https://www.apa.org website: https://www.apa.org/topics/trauma
Center for Child Trauma Assessment and Service Planning. (2015). What is trauma-focused therapy? Retrieved from: http://cctasi.northwestern.edu/family/trauma-focused-therapy/
Wu, J. (2017). Attachment, self-regulation, and competence: A comprehensive framework. Retrieved from: https://www.nctsn.org/interventions/attachment-self-regulation-and-competence-comprehensive-framework
Wu, J. (2017). Cognitive-behavioral intervention for trauma in schools. Retrieved from: https://www.nctsn.org/interventions/cognitive-behavioral-intervention-trauma-schools